How Long Does a Dental Cleaning Take?
Dental cleanings are essential preventative procedures used to maintain your oral health by decreasing the risk of tooth decay and gum disease. The American Dental
Dental cleanings are essential preventative procedures used to maintain your oral health by decreasing the risk of tooth decay and gum disease. The American Dental
Family dentists are concerned with helping your entire family take care of their teeth and they offer many preventative dentistry services. These services are intended
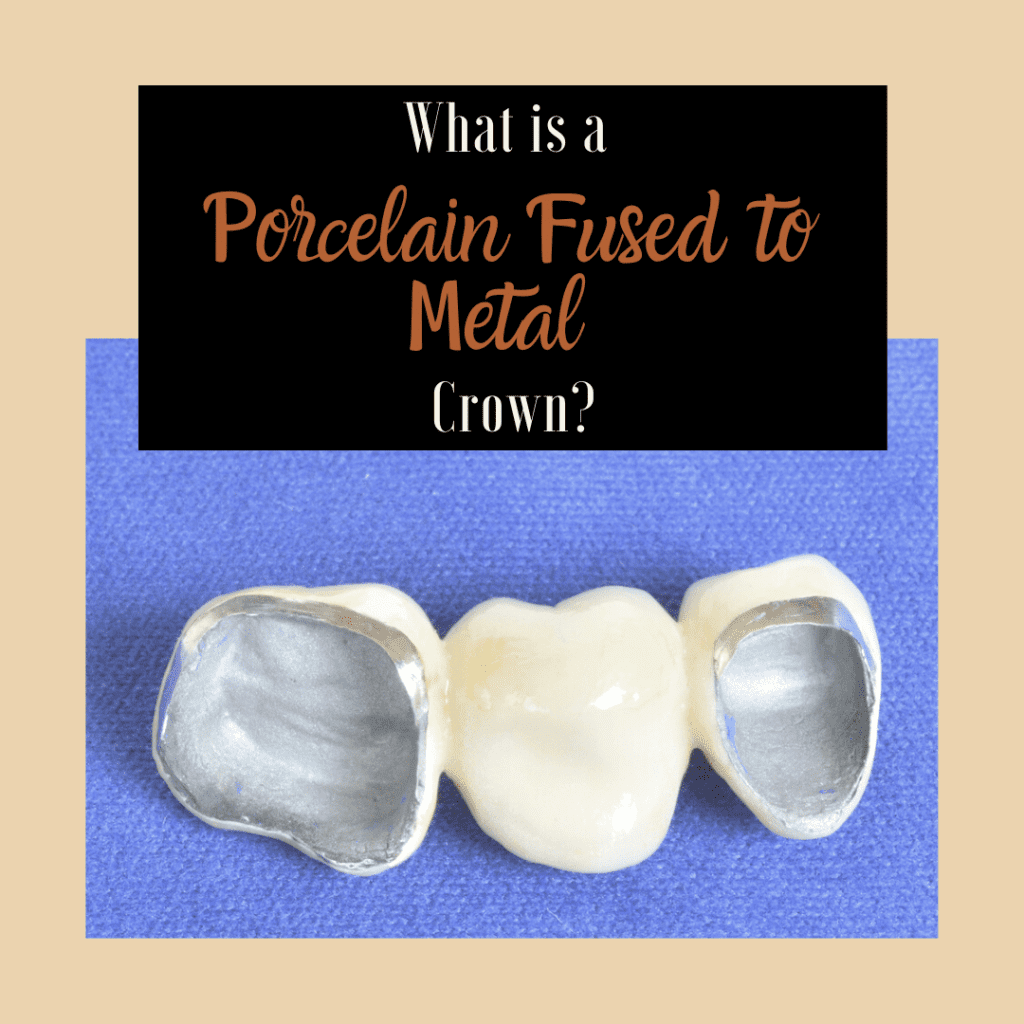
If you have a tooth that is chipped, cracked, or decayed, your dentist will likely recommend a dental crown to protect the remaining tooth structure
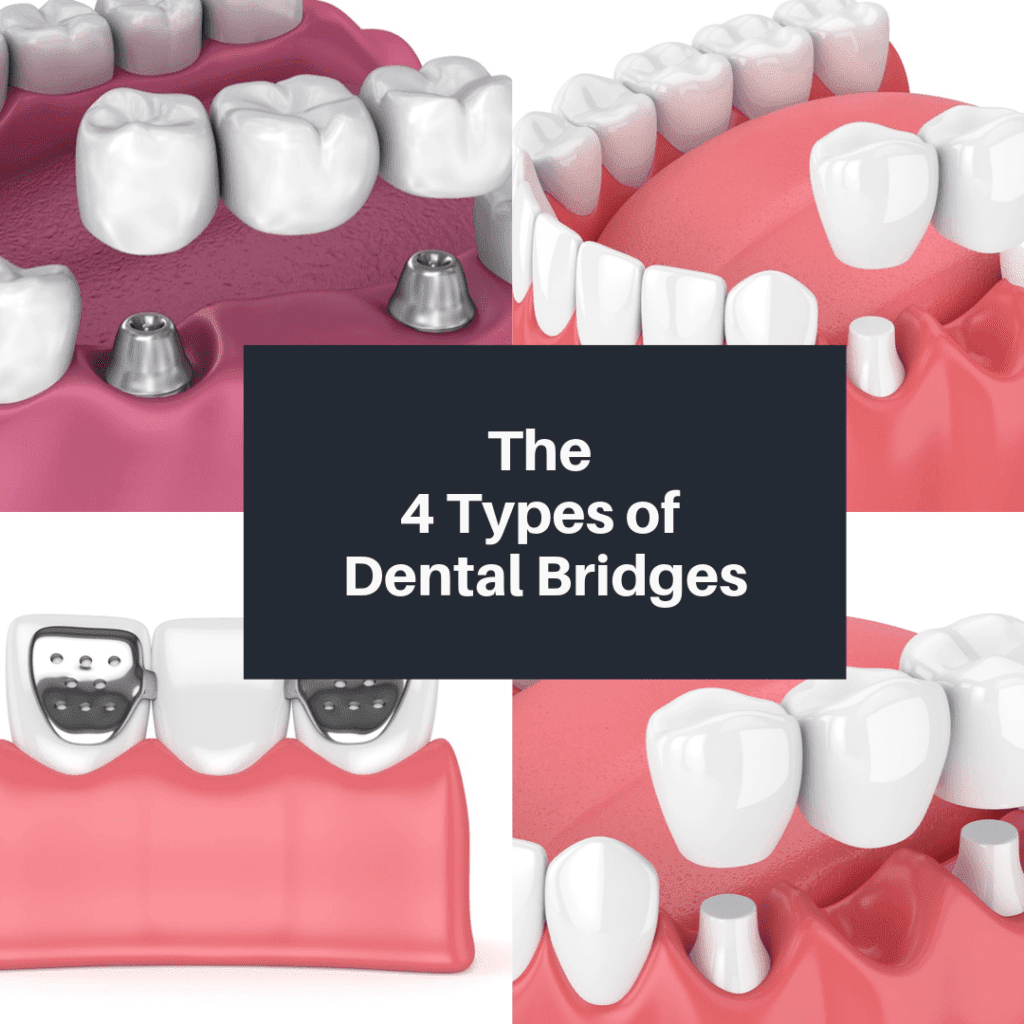
Whether you’ve lost a tooth from past dental trauma or due to decay or damage, any dentist will tell you that it is important to
Although the term “dental crown” makes it sound like a tiny crown for your tooth, dental crowns are caps that fit over the tooth. Dental
Besides preserving your oral health, one of the main goals of modern dentistry is to make dental procedures as comfortable as possible. With the introduction

General dentistry is the practice of providing dental services that identify, diagnose, treat, and prevent dental issues. Because of their expansive skillset, general dentists can

It is no secret that modern dentistry can be expensive. Often, the cost of dental treatments is one of the main obstacles preventing people form

The American Dental Association recommends visiting your dental office every six months. Busy lives and minor dental anxiety can cause many people to wonder if

Did you know that part of your dental checkup at Pasha Dental deals with having an oral cancer screening? You may be wondering why it